Corneal diseases are a major
cause of blindness, second only to cataract in overall importance1.
Furthermore, persons with corneal blindness are of a younger age group compared
with those suffering from cataract. Therefore, in terms of total blind years,
the impact of corneal blindness is greater. The cornea is a virtually avascular
tissue, but it has very dense innervation (40 times more than the
tooth pulp and 400 times more than skin)2.
Nerve growth factor plays a special role in growth and
differentiation of peripheral sensory nerve cells and help in repairing the
damaged nerve fibers3. Thus,
any inflammatory reaction and subsequent healing are controlled by
this neuronal innervation4. Corneal sensitivity threshold is
significantly higher in male than female (females more sensitive). Reduction in
corneal threshold (increase in sensitivity) occurs with age in females but not
males5. Corneal nerves damage impairs epithelial healing
and induces trophic keratopathy even in the absence of
injury or infection6. According to Mackie classification7,8,
neurotrophic keratopathy is divided into three stages. Stage 1: is dry eye, with resultant vascularization and scarring
of cornea. Stage 2: is non
healing corneal epithelial defect. Stage
3: is stromal melting leading to perforation. Treatment of neurotrophic
keratopathy at stage 1 is therefore necessary to prevent further complication,
and to restore corneal function. Unfortunately available treatments do not help
the patient to the level of their satisfaction.
Several
ocular and systemic diseases, including fifth-nerve palsy, viral
infections, chemical burns, corneal surgery, abuse of topical
anesthetics, diabetes mellitus, leprosy, and multiple sclerosis, can cause
sensory-nerve impairment8. Loss of corneal sensation leads to a
decrease in the number of corneal stem cells9, decreased
metabolic and mitotic rates in the corneal epithelium10.
The result is progressive corneal damage with epithelial defects, vascularization,
stromal scarring, ulceration, and ultimately perforation even in the
absence of injury or infection. In viral keratitis interaction with host
immunity results in corneal opacity11.
The
standard treatment of corneal opacity is expensive, often ineffective,
and the outcome may be loss
or severe impairment of vision. New drug modalities such as epidermal growth
factor, nerve
growth factor, fibroblast growth factor (FGF-2), vascular endothelial
growth factor etc have been found effective in achieving normal corneal
integrity. Majority of these growth factors are present in the human milk
including NGF12. Growth factor activity is present
throughout the lactation period in the human milk but in bovine milk
only during the colostral phase13.
Human breast milk is still in
use as Traditional Eye Medicine (TEM) for corneal ulcer in rural areas.
However, no clinical research has been conducted so far to see its beneficial
or adverse effects on the human eye. This study will therefore be the first of
this nature.
MATERIAL AND METHODS
Before
treatment, informed consent was taken from all the patients. Dignity, honor,
and privacy of patient and the human milk provider were always maintained. Observational
clinical analysis was then carried out on patients of either sex having corneal
opacity accompanied with decreased corneal sensitivity and negative
conjunctival swab culture. Patients having neurotrophic corneal opacity due to
viral keratitis (Mackie classification stage 1), long standing disciform
keratitis, recurrent viral keratitis and long standing diabetes with
neurotrophic cornea were registered for study. Initial examination was
performed in outpatient department. After getting informed consent, detailed
history was taken which included; age, sex, residency, occupation, any previous
history of trauma to eye, and socioeconomic condition. The data was also
collected related to any surgery which can damage trigeminal nerve, topical
medication, corneal surgery, associated systemic disease and family history.
Best – corrected
visual acuity was noted using Snellen’s chart. Slit lamp examination of normal
and affected eye was done, and where possible dilated indirect ophthalmoscopy
with 90D was also performed. Corneal staining of affected eye was done to rule
out active ulcer, for which one drop of fluorescein 1% was used. The corneal
opacity was examined for size, site, density, location and invasion of blood
vessels. All layers of cornea and anterior chamber were examined carefully on
slit lamp. Corneal sensitivity was tested with cotton tip at the center of the
cornea of affected eye. When the cornea was touched with cotton tip, the
sensitivity was considered normal if a blink reflex was present. If
the patient felt contact but had no blink reflex corneal hypoesthesia
was diagnosed, and if no response was present corneal anesthesia was
diagnosed. Corneal/ conjunctival sensitivity to chemical stimulation
was also determined by noting a burning sensation after conjunctival
instillation of a pungent substance in the affected eye of patient14
for which Naclof (diclofenac sodium) eye drops were used in the affected eye.
Short term use of non steroidal anti-inflammatory drugs (NSAID)
are harmless to ocular surface and do not decrease corneal sensitivity and tear
secretion15.
Intraocular
pressure was checked with air puff tonometer in both eyes. Conjunctival swab
sampling, culture, and random blood glucose assessment was performed by the
pathologist in the laboratory.
The
patients were then put on topical human milk four times daily. Every patient
requested the healthy nursing woman at his or her home or any other nursing
woman for fresh milk four times daily. The milk was taken in a clean stainless
steel spoon and used by the patient with the help of sterilized dropper immediately.
Topical tobramycin 0.3% ophthalmic drops were also used four times daily to
prevent bacterial infection.
Follow up was done on day 7,
day 15, and then every month up to 6 months. On every follow up visit complete
assessment including visual acuity, size and thickness of corneal opacity,
corneal sensitivity, and any complication was noted. Same research protocol was
used by all the authors and all patients were discussed online to maintain
uniformity.
SPSS 14.0 (Statistical Package
for Social Sciences) was used for statistical analysis. Paired t-test was used
to assess visual acuity in numbers of eyes before and after treatment with
human milk in patients with diabetic neurotrophic and viral neurotrophic
corneal patients. For data analysis visual acuity was used in decimals. Mean
visual acuity before management was 0.2 and after management was 0.7,
independent sample test was performed to see significant difference between two
groups. There was significant difference in visual outcome between viral and
diabetic neurotrophic corneal opacity patients, P value 0.004.
RESULTS
Out of 43 recruited patients of neurotrophic corneal opacity, only
40 patient completed full follow up of six months. Three patients with
incomplete follow up were dropped from study. Among these 40 patient 16 were
diabetic and 24 with previous viral keratitis. Majority of these patients were
from rural areas and most of them were poor. Most of these patients were
previously treated with acyclovir due to decreased corneal sensitivity (table 1).
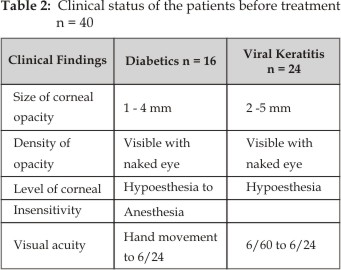
These patients had either central or paracentral corneal opacity
which was visible with naked eye (Figure 1 and 2) and reduced corneal
sensitivity. Size of corneal opacity ranged between 2 to 5 mm. In diabetic
patients skin sensitivity was also affected on the extremities along with
corneal sensitivity but in viral patients peripheral skin sensation was normal.
Best corrected visual acuity ranged between hand movements to 6/24 before
treatment (table 2).
Table 1: Bio-data of patients
|
Total recruited patients |
43 |
|
Dropped from study (incomplete follow up) |
03 |
|
Patients completed follow up of 6 months |
40 |
|
Male |
26 |
|
Female |
14 |
|
Age |
20 to 55 years |
|
Diabetic more than 10 years |
16 Patients |
|
Previous Viral keratitis |
24 Patients |
|
Socioeconomic condition |
Middle and lower class |
|
Residency |
32 Rural 8 urban |
|
Past medical history |
acyclovir eye ointment |
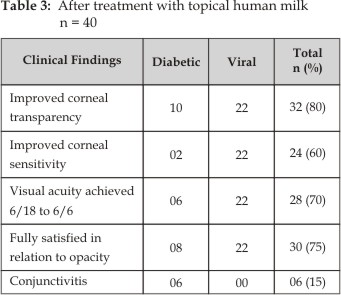
Response to treatment was observed within 15 days following
topical use of human milk. Viral induced neurotrophic corneal opacity responded
much better than diabetic neurotrophic opacity. 32 patients (80%) achieved
nearly complete transparency of cornea within 30 to 90 days of treatment
(figure 3 and 4). Corneal sensitivity improved in 24 (60%) eyes and reported a
burning sensation after conjunctival instillation of Naclof
(diclofenac sodium) eye drops. Eight patients in whom corneal
clarity occurred without significant improvement in sensitivity were diabetic. Best
corrected visual acuity improved in 28 (70%). Visual acuity did not improve in
two diabetic patients due to cataract although cornea became clear. Transient
conjunctival hyperemia was noted in nearly all cases during initial
treatment. 8 (20%) patients did not
respond completely. Bacterial conjunctivitis occurred in 6 (15%) patients which
recovered with frequent use of tobramycin eye drops. Post-treatment findings
are given in table 3. Complications were mostly encountered in diabetic and
malnourished patients.
The mean duration of treatment
was 55 days. The first sign of good response on slit lamp
examination was reduction in scar size in subepithelial layers (bowman’s and
stroma). Feeling of burning to Naclof
eye drops was also noted. Burning sensation indicates recovery of corneal
sensation. These ocular findings gradually disappeared and cornea became
completely clear. The improvements in corneal
sensitivity and visual acuity were maintained throughout the
follow-up period. None of the patients had systemic side effects
during treatment with human milk. Moreover, none had a
relapse of their eye disease during follow-up.

Fig. 1: Central corneal opacity.

Fig. 2: Clear cornea after treatment

Fig. 3: Before treatment

Fig: 4: after treatment
DISCUSSION
Persistent
corneal epithelial defects due to decreased corneal sensitivity result in
corneal scarring, neovascularisation, and decreased vision. Threshold corneal
sensitivity level is required which can maintain anatomical and functional
integrity of cornea16. Many
ocular and systemic conditions provoke a loss in corneal sensitivity sufficient
to alter anatomical and physiological integrity of cornea: surgical treat-ment
of trigeminal neuralgia and acoustic neuroma, ocular viral infection, diabetes,
corneal graft, LASIK, chemical burns, multiple sclerosis, local anesthetics and
anti-inflammatory medication, contact lenses, familia dysautonomia. It is not
possible to reverse corneal sensory loss in all these conditions, however
corneal sensitivity can be improved where the cause of sensory loss is viral,
contact lens, or local anesthetic.
Topical use of growth factor, sensory
neurotransmitter or human milk cannot restore corneal sensory loss in systemic
disease with17 generalized neuropathy, however local neurotrophic
corneal opacity do respond to topical treatment; with human milk, individual
growth factor, or neurotransmitter which is deficient in neurotrophic cornea. The
effect of NGF is mediated through TrkANGFR
and p75NTR receptors18. Several studies showed that loss
of NGF receptor TrkANGFR (tropomyosin receptor kinases) develop corneal opacity and impairment of corneal
sensitive nerves.
Human milk contains nerve growth factor in reasonable
concentration which is maintained throughout the lactational period. Lactoferrin
plays an important role in the defense against infections, inclu-ding herpes
simplex virus (HSV) keratitis19. Lacto-errin is an iron binding
protein. It is very abundant in colostrum. Lactoferrin can inhibit viral
infection by binding tightly to the viral envelope protein.
Neurotrophic
cornea is usually accompanied by a reduction of tears or a reduced blinking of
the lids which further aggravates the condition. Human milk contains not only growth
factors and lactoferin but also tear components, like fat water and
electrolytes, which helps in maintaining tear film. Human milk therefore covers
all aspects of the problem.
We have
found human milk very effective in eliminating corneal opacity associated with
corneal hypoesthesia. These are the growth factors and lactoferrin in the human
milk which play important role in the elimination of neurotrophic corneal scar.
Nutritional factors in the human milk may also have positive effect in this
process. However extent of response to human milk varies from patient to
patient depending on cause of neurotrophic corneal opacity,
age and general health of the patient.
Human
milk therefore, inhibits viral infection, clears corneal opacity, improves
corneal sensitivity, and restores corneal integrity with minimal complications
and little expense. Human milk contains significantly more lactose, even more
than cow's milk and this may also stimulate the growth of microorganisms20
but this can be prevented by topical use of antibiotic (tobramycin 0.3%).
During treatment some patients had photophobia and
burning of their eyes during slit-lamp examinations, which suggests
functional recovery of corneal innervation. The maintenance of corneal
sensitivity after treatment with human milk suggests that such treatment
completely restores sensory innervation of the cornea mainly in
viral patients.
Conjunctivitis was main side effect reported during the treatment.
No relapse of the disease was observed during the follow-up period in the
patients who responded to treatment, but relapse is possible in neurotrophic
cornea due to systemic disease, as in diabetes.
Because
no other study has been so far conducted directly on human milk therefore
results cannot be compared with other studies, however individual growth
factors like epidermal growth factor21, nerve growth factor22,
and vascular endothelial growth factor23 are effective in
neurotrophic keratopathy. Our results are comparable with nerve growth factor
which restores corneal integrity.
CONCLUSION
Human milk is effective in
restoring corneal transparency in neurotophic corneal opacity, especially in
viral neurotrophic cornea, if risk of bacterial infection is controlled with
topical antibiotics. The treatment is easy to use, available everywhere, and
cost effective especially in developing country. However we do not recommend
its use until the facts are fully established by case and control study. The
results can be improved further by using bensalkonium chloride free antibiotic
and good nutrition for malnourished patients.
Author’s Affiliation
Dr. Munawar Ahmed
Assistant professor
Department of ophthalmology
Liaquat University of Medical and Health Sciences
Jamshoro
Dr. Muhammad Saeed
Associate professor
Department of Ophthalmology
Azra Naheed Medical College
The
Superior University Lahore
Dr. M. Arshad Mahmood
Associate Professor
Department of Ophthalmology
University College of Medicine & Dentistry
The University of Lahore
REFERENCES
1.
Oliva MS,
Schottman T, Gulati M. Turning the tide of corneal blindness Indian
J Ophthalmol. 2012; 60: 423-7.
2.
Bonini S, Lambiase
A, Aloe L, Mantelli F, Sacchetti M, Rocco ML. Capsaicin-induced
corneal sensory denervation and healing impairment are reversed by NGF
treatment. Invest. Ophthalmol. Vis.
Sci, 2012; 53: 8280-7.
3.
Levi-Montalcini R. The nerve growth factor 35 years later. Science.
1987; 237: 1154-62.
4.
Tervo K, Latvala TM, Tervo TM. Recovery of corneal innervation
following photorefractive keratoablation. Arch Ophthalmol. 1994; 112: 1466-70.
5.
Golebiowski, Blanka Boptom, Papas, Eric
B, Faao; Stapleton, Fiona Mcoptom. Faao Factors affecting corneal and conjunctival sensitivity
measurement Optometry and Vision Science. 2008; 85: 241-6.
6.
Price FW Jr, Whitson WE, Marks RG. Graft survival in four common groups
of patients undergoing penetrating keratoplasty. Ophthalmology. 1991; 98:
322-8.
7.
Groos, E. Cornea,
2004; 94: 1189–1196.
8.
Mackie IA. Neuroparalytic
keratitis. In: Fraunfelder FT, Roy FH, eds. Current ocular therapy, Philadelphia W.B. Saunders; 1995:
506-8.
9.
Puangsricharern V, Tseng SCG. Cytologic evidence of corneal diseases
with limbal stem cell deficiency. Ophthalmology. 1995; 102: 1476-85.
10.
Sigelman S, Friedenwald JS. Mitotic and wound-healing activities
of the corneal epithelium: effect of sensory denervation. Arch Ophthalmol.
1954; 52: 46-57.
11. Shtein RM, Elner VM. Herpes simplex virus keratitis: histopathology and corneal allograft
outcomes Expert Rev
Ophthalmol. 2010; 5: 129-34.
12.
Gaull
GE, Wright CE, Isaacs. Significance of growth modulators in human milk pediatrics. 1985; 75:
142-5.
13. YW Shing, M
Klagsbrun Human and bovine milk contain
different sets of growth factors. Endocrinology.
1984; 115:273-82.
14.
Faulkner WJ, Varley GA. Corneal diagnostic technique. In: Krachmer JH,
Mannis MJ, Holland EJ. Cornea:
fundamentals of cornea and external disease. St. Louis: Mosby–Year Book, 1997: 275-81.
15.
Yanai K, Huang J, Kadonosono K, Uchio E. Corneal
sensitivity after topical bromfenac sodium eye-drop instillation Clinical
Ophthalmology. 2013; 7: 741-4.
16.
Dogru M, Yildiz M, Baykara M, Ozçetin H, Erturk H. Corneal sensitivity and ocular surface changes following preserved
amniotic membrane transplantation for non healing corneal ulcers Eye. 2003; 17:
139-48.
17.
Nishida, Teruo, Yanai, Ryoji. Advances in treatment for neurotrophic
keratopathy Current Opinion in Ophthalmology. 2009; 20: 276-81.
18.
You L, Kruse FE, Hans E. Volcker Neurotrophic Factors in Human Cornea Investigative
ophthalmology and visual science. 2000; 41: 692-702.
19.
Keijser S, Jagar
MJ, Dogterom – Ballering, Schoonderwoerd, Krose, JJ. Houwing
– Duistermaat. Lactoferrin Glu561Asp
polymorphism is associated with susceptibility to herpes simplex keratitis.
Experimental eye research. 2008; 86: 105-9.
20.
Prajna VN, Pillai MR, Manimegalai TK, Srinivasan
M. Use of
traditional eye medicines by corneal ulcer patients presenting to a hospital in
South India Indian Journal of Ophthalmology. 1999; 47: 15-8
21.
G Carpenter. Science promoting agent in breast milk.
Science, 1980; 210: 198-9.
22.
Lambiase A, Rama P, Bonini S,
Caprioglio G, Aloe L.
Topical treatment with nerve growth factor for corneal neurotrophic ulcers. The
New England journal of medicine, 1998;
17: 1174-80.
23.
Yu CQ, Zhang M,
Matis KI, Kim C, M. I. Rosenblatt. Investigative Ophthalmology and Visual Science. 2008; 49: 3870-8.